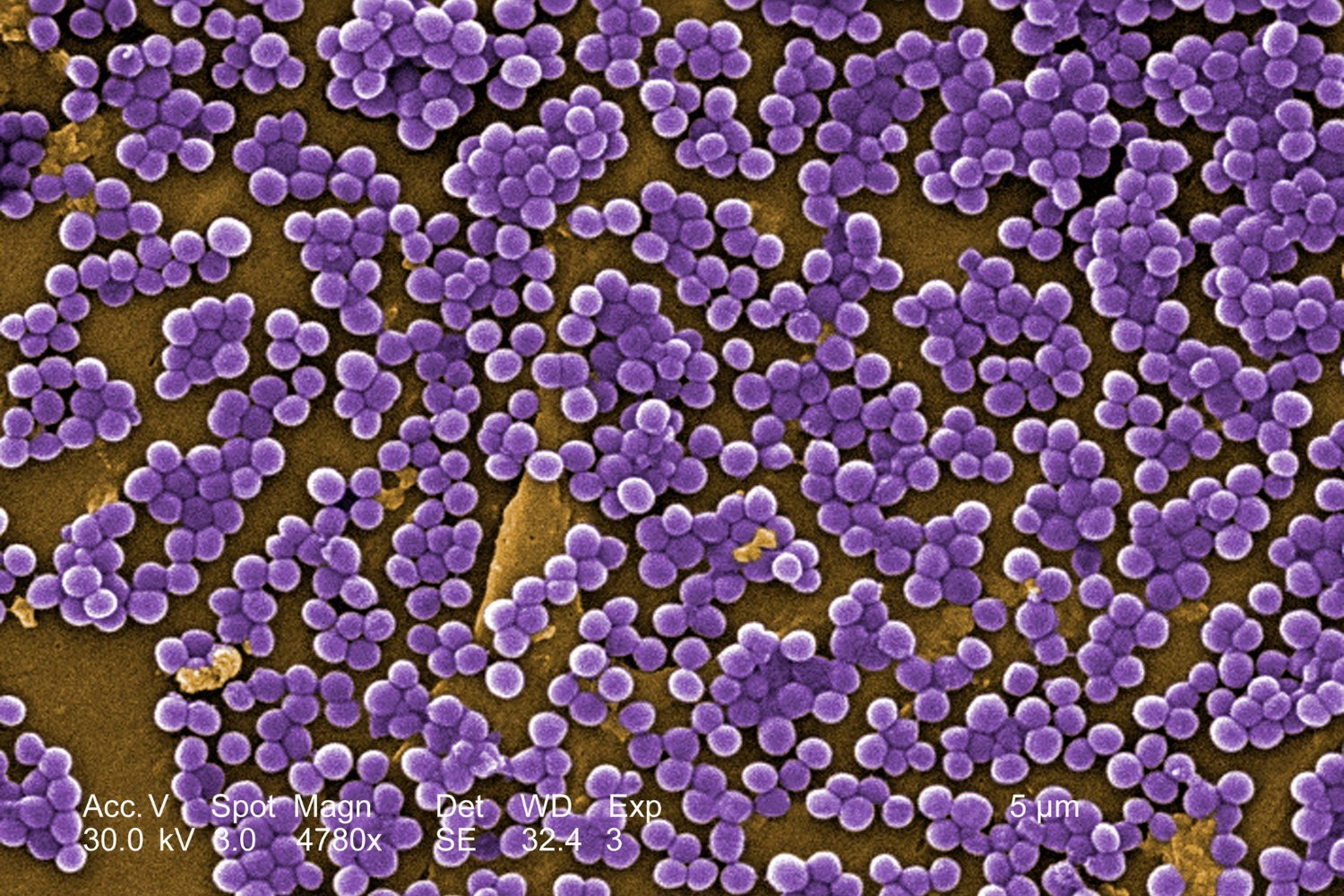
Drug-resistant bacterial infections, often called superbugs, pose a significant threat to global health. A recent report estimates these infections could directly cause over 39 million deaths in the next 25 years, contributing to nearly nine million deaths annually by 2050. Without substantial intervention, the impact of antimicrobial resistance (AMR) could be devastating.
This alarming projection comes from the Global Research on Antimicrobial Resistance (GRAM) Project, a collaboration between the University of Oxford and the University of Washington’s Institute for Health Metrics and Evaluation (IHME). Funded by organizations like the Wellcome Trust and the Bill & Melinda Gates Foundation, GRAM researchers analyzed a massive dataset of 520 million records, including hospital data and antibiotic usage patterns, spanning 204 countries. Their analysis encompassed 11 broad infection types, 22 specific pathogens, and 84 unique pathogen-drug interactions across all age groups.
GRAM’s research reveals a concerning trend. From 1990 to 2021, drug-resistant infections directly caused over one million deaths annually, with a slight increase from 1.06 million in 1990 to 1.14 million in 2021. These infections also contributed to nearly five million deaths each year during this period. While a slight dip was observed in 2021 compared to 2019, this is likely attributed to the COVID-19 pandemic and its associated social distancing measures, which temporarily reduced the spread of many infectious diseases. Encouragingly, superbug-related deaths in children under five decreased by 50% between 1990 and 2021, a trend projected to continue. However, overall deaths, especially among older and vulnerable populations, are expected to rise.
Looking ahead, the GRAM study paints a grim picture. Between 2025 and 2050, drug-resistant infections are projected to directly kill over 39 million people, with an estimated 1.91 million deaths in 2050 alone. These superbugs will further contribute to nearly 170 million deaths during this timeframe, reaching 8.22 million in 2050. The burden of AMR won’t be evenly distributed, with South Asia projected to bear the brunt, accounting for a quarter of all direct deaths (11.8 million). Other parts of Asia and sub-Saharan Africa are also expected to experience high death tolls.
These findings align with previous estimates, such as a 2014 UK government report that projected up to 10 million deaths from drug-resistant infections by 2050. If these predictions hold true, superbugs could eventually surpass cancer as a leading cause of death.
While promising new antibiotics are on the horizon, offering hope against drug-resistant strains of gonorrhea and other common superbugs, and incentives for antibiotic research and development are showing some success, the GRAM researchers emphasize the need for more aggressive action. Without significant interventions, the worst-case public health scenarios could become reality.
Timothy Jinks, Head of Interventions in Wellcome Trust’s Infectious Disease team, stresses the urgency of the situation. While acknowledging recent progress in tackling AMR, he underscores the need for intensified efforts. The GRAM estimates serve as a critical tool in this fight, providing evidence for policymakers to make informed decisions. Bold action against AMR is crucial to strengthening health systems and safeguarding vulnerable populations from the devastating impact of infectious diseases.