Hospital sink drains can be a reservoir for drug-resistant bacteria, even with rigorous cleaning protocols, according to a new study. This discovery underscores the challenges in combating the spread of superbugs within healthcare settings.
Antibiotic resistance poses a significant global health threat. The Centers for Disease Control and Prevention (CDC) estimates that drug-resistant infections cause at least 1.27 million deaths globally each year, including 35,000 in the United States. Projections suggest these infections could surpass cancer as a leading cause of death in the coming decades. Hospitals, with their widespread use of antimicrobials and concentration of vulnerable patients, are particularly susceptible to the spread of these resistant bacteria. Despite regular deep cleaning procedures aimed at mitigating this risk, the new study highlights the persistence of these dangerous pathogens.
Persistent Bacterial Communities in Hospital Drains
The study, published in Frontiers in Microbiology, investigated the bacterial populations within sink drains of a well-maintained university hospital on the island of Majorca. The hospital employs stringent cleaning protocols, including regular bleach cleaning, bi-weekly disinfection with pressurized steam and chemicals, and annual chlorine treatment of the piping system. Researchers collected bacterial samples from six sink drains across five wards (two ICUs, hematology, short stays, general medicine, and a microbiology lab) over a year, from February 2022 to February 2023.
Diverse and Resistant Bacteria Thrive
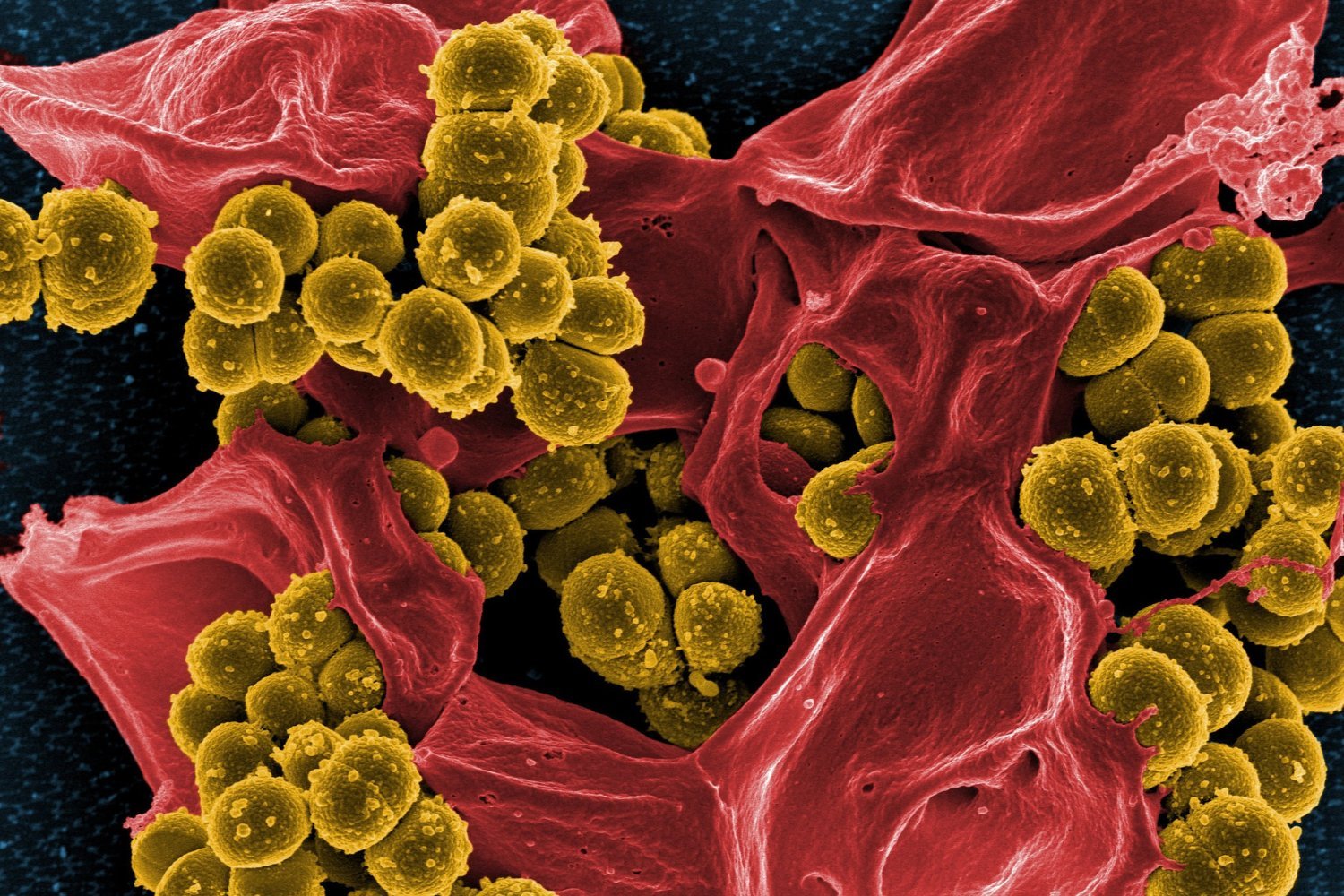
Genetic sequencing revealed 67 different bacterial species across the drains. While some variation existed between wards, all drains harbored a diverse range of bacteria, including common culprits of hospital-acquired infections like Pseudomonas aeruginosa, Klebsiella pneumoniae, and Staphylococcus aureus. Surprisingly, the established cleaning procedures appeared to have minimal impact on the overall bacterial diversity. Even a newer ICU unit, operational for only a year prior to the study, showed similar bacterial colonization.
Antibiotic Resistance and Carbapenem-Resistant Genes
Alarmingly, many samples contained bacteria resistant to multiple antibiotics, particularly strains of P. aeruginosa and K. pneumoniae. Researchers also identified a gene associated with resistance to carbapenems, a class of last-resort antibiotics, raising significant concerns. This suggests that hospital sink drains may not only harbor resistant bacteria but also contribute to the spread of resistance genes.
Rethinking Infection Control Strategies
While the study emphasizes the importance of continued cleaning protocols, it also underscores the need for a more comprehensive approach to infection control. Understanding the origins of these bacteria and their transmission routes within the hospital environment is crucial for developing effective strategies to combat the spread of antibiotic resistance. Further research is needed to explore alternative disinfection methods and investigate the potential role of sink drain architecture in bacterial colonization.
The Need for Comprehensive Solutions
This study highlights the ongoing challenge of combating antibiotic resistance in healthcare settings. While meticulous cleaning remains essential, it alone is insufficient to eliminate the threat posed by drug-resistant bacteria lurking in hospital sink drains. A multi-faceted approach, combining improved cleaning protocols with a deeper understanding of bacterial ecology and transmission dynamics, is necessary to protect vulnerable patients and curb the rise of superbugs.