When evaluating options for significant weight loss, new research underscores that bariatric surgery continues to deliver more substantial results compared to the latest GLP-1 medications for obesity. A recent study from New York University, analyzing real-world patient data, found that individuals undergoing surgical weight loss procedures lost considerably more weight than those prescribed GLP-1 drugs. This research also suggests a potential gap between the effectiveness of GLP-1 drugs in controlled clinical trials and their performance in everyday settings.
The study revealed that, on average, surgical patients lost five times more weight over a two-year period compared to those using GLP-1 agonists. “I think the takeaway is when you see a new popular drug come out, you have to take it with a grain of salt. And I think you have to wait a few years for the real world data to come out, because it might temper the results you’re seeing in trials,” senior study researcher Karan Chhabra, a bariatric surgeon and assistant professor of surgery and population health at the NYU Grossman School of Medicine, told maagx.com.
The Established Efficacy of Bariatric Surgery
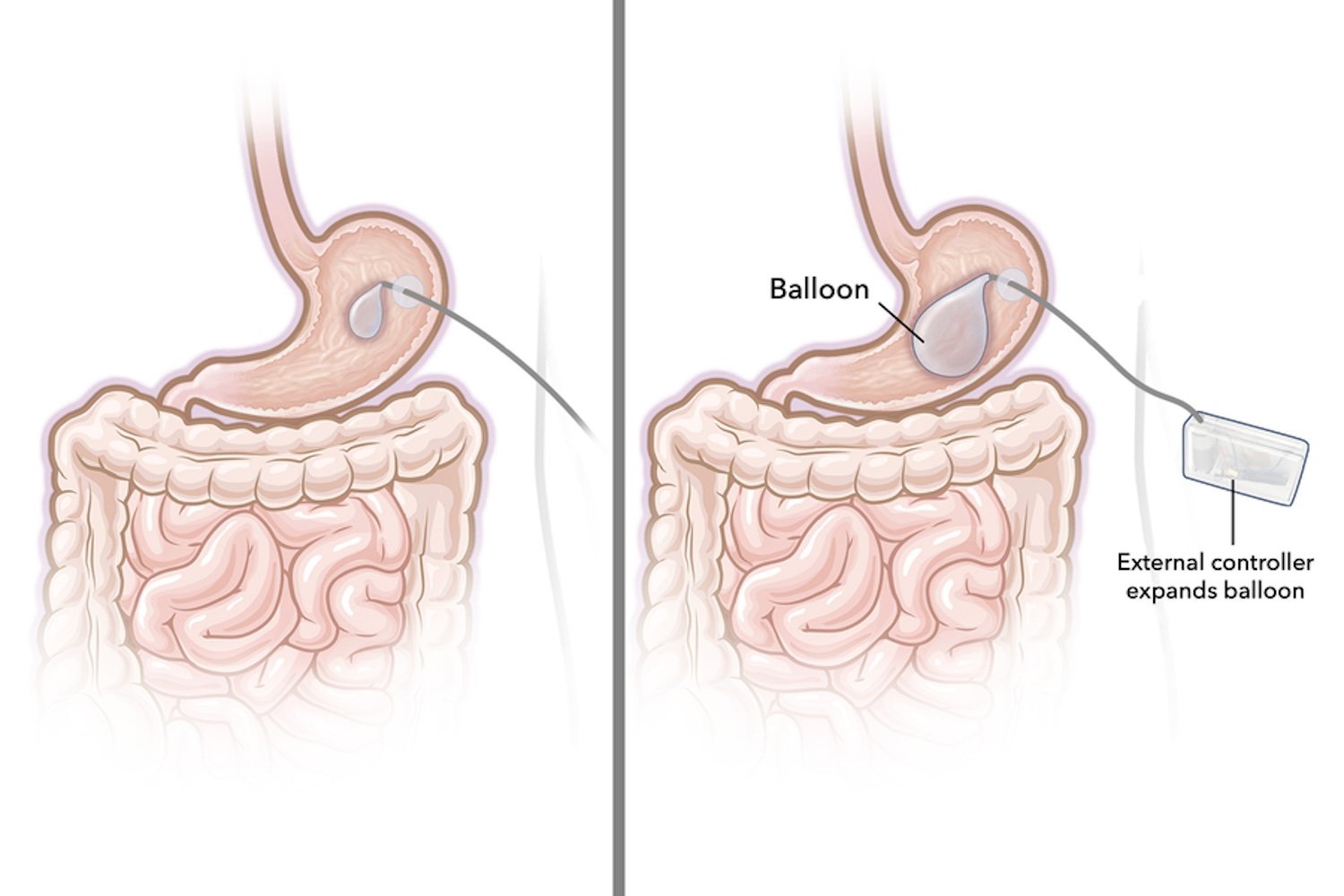
Bariatric surgery, encompassing procedures like the sleeve gastrectomy and gastric bypass, has long been recognized as the most potent treatment for severe obesity. Typically, patients achieve a weight loss of 20% to 30% of their initial body weight following these surgical interventions. Beyond weight reduction, these procedures often lead to sustained improvements in overall health, addressing obesity-related comorbidities.
The Ascent of GLP-1 Agonists in Obesity Medicine
In recent years, the landscape of obesity medicine has been significantly reshaped by the introduction of newer GLP-1 receptor agonists, such as semaglutide (marketed as Ozempic and Wegovy) and tirzepatide. These medications have demonstrated greater efficacy and a better safety profile compared to previous non-surgical obesity treatments. Clinical trials have shown average weight loss ranging from 10% to 20% with these drugs, along with associated health benefits that extend beyond mere weight reduction. Initial data even suggested that GLP-1 drugs might rival or exceed the effectiveness of bariatric surgery. However, Dr. Chhabra pointed out the absence of rigorous, direct comparisons between these two treatment modalities among real-world patients until now.
A Real-World Showdown: Study Design and Findings
To address this gap, Dr. Chhabra and his colleagues embarked on a comprehensive comparative study.
Study Methodology and Scope
The research team analyzed the anonymized medical records of over 50,000 individuals. These patients had either undergone bariatric surgery (sleeve gastrectomy or gastric bypass) or received GLP-1 therapy (semaglutide or tirzepatide) through NYU Langone Health or NYC Health + Hospitals between 2018 and 2024. To ensure a fair comparison, the researchers meticulously adjusted for various factors, including age, initial Body Mass Index (BMI), and co-existing health conditions. The weight loss trajectories of these patients were then monitored for a two-year period.
Key Findings: Surgery Outperforms GLP-1s Significantly
The results were striking. By the end of the two-year follow-up, patients who had bariatric surgery lost an average of 58 pounds, equating to approximately 24% of their total body weight. In contrast, patients on GLP-1 medications lost an average of 12 pounds, or about 4.7% of their total body weight. This represents a fivefold greater weight loss with surgery.
Even when considering patients who adhered to their GLP-1 medication for a full year, their average weight loss was 7%. Those taking tirzepatide, the newest and generally most effective GLP-1 drug currently available, achieved an 8% to 9% weight loss. While these figures are improvements, they still fall significantly short of the outcomes seen with bariatric surgery and are notably lower than the results reported in earlier clinical trials.
The team’s findings were presented at the annual meeting of the American Society for Metabolic and Bariatric Surgery (ASMBS).
Unpacking the Discrepancy: Why Real-World GLP-1 Results Differ
Dr. Chhabra highlighted several potential reasons for the observed disparity between clinical trial data and real-world effectiveness of GLP-1 drugs.
High Discontinuation Rates and Side Effects
A significant factor is the high rate of discontinuation among GLP-1 users; as many as 70% of patients stop using these medications within the first year. Common reasons for discontinuation include intolerable side effects, which are typically gastrointestinal issues such as nausea and diarrhea.
Cost and Accessibility Challenges
The substantial cost of GLP-1 medications is another major barrier. These drugs are often not covered by insurance and can cost over $1,000 per month out-of-pocket, making long-term adherence financially unfeasible for many. The study also noted that many GLP-1 patients never reached the maximum therapeutic dose, potentially limiting efficacy.
Lack of Comprehensive Supportive Care
Dr. Chhabra also suspects that real-world patients often do not receive the same level of supportive care and consistent follow-up from healthcare providers as participants in a structured clinical trial. The rise of telemedicine has facilitated remote prescribing of GLP-1 drugs, sometimes by medical professionals with whom patients have no personal interaction. Furthermore, until recently, compounded versions of semaglutide and tirzepatide were more readily available, often with less assurance regarding their safety or consistent effectiveness. [internal_links]
Navigating Treatment Choices: Important Considerations for Patients
The researchers emphasize that their findings do not mean individuals with obesity should avoid GLP-1 drugs, nor do they suggest that bariatric surgery is the universal ideal choice. Patient preferences and circumstances vary widely. Some individuals may prefer a one-time surgical intervention, while others might lack the insurance coverage or financial resources for sustained GLP-1 therapy. Conversely, some patients may be apprehensive about undergoing an invasive procedure or have pre-existing health conditions that could make surgery riskier, whereas GLP-1 therapy might be a safer alternative for them.
Ultimately, individuals considering weight loss treatments need to be fully informed about the respective advantages and disadvantages of each option. Dr. Chhabra advises that those opting for GLP-1 medications should have realistic expectations regarding potential outcomes.
“They have to know that, at least as of now in the real world, their weight loss is not going to be what we’re seeing with surgery and they also have to know that it’s a lifelong treatment,” he stated. “We don’t yet have any protocols for people to maintain weight loss once they’ve stopped medications so it’s important for people to just acknowledge those realities. And I worry that a lot of people are starting medications without really knowing what they’re getting into.”
The research team plans to delve deeper into their data to better understand the specific factors contributing to the lower-than-expected weight loss among real-world patients on GLP-1 therapy. This ongoing investigation aims to provide further clarity for both patients and clinicians in the evolving field of obesity treatment.
References
- The team’s findings were presented this week at the annual meeting of the American Society for Metabolic and Bariatric Surgery (ASMBS).