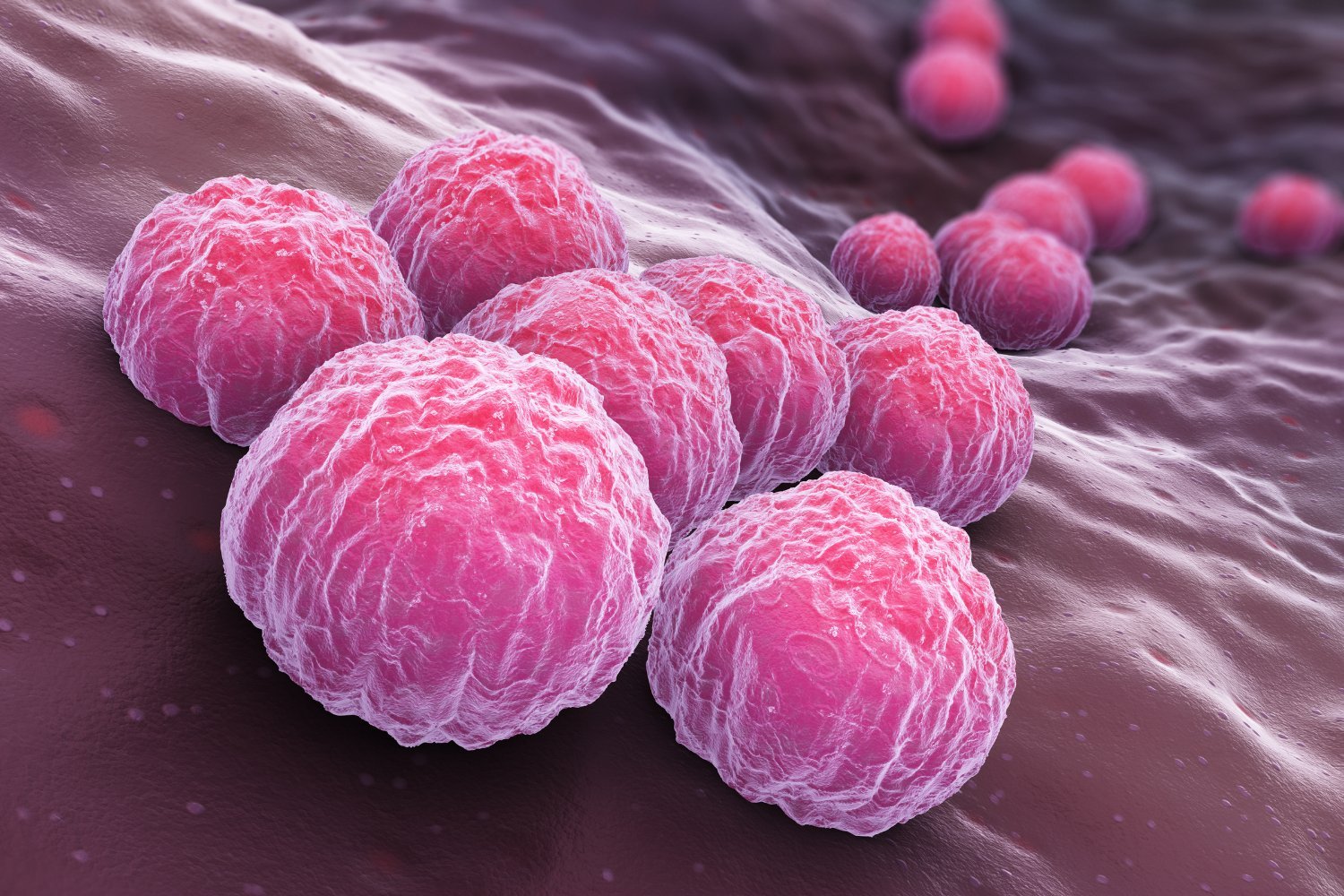
Chlamydia, a common sexually transmitted infection (STI), may be more complex than previously thought. New research suggests the bacteria responsible, Chlamydia trachomatis, may be able to hide in the human gut, potentially explaining recurring infections even after successful antibiotic treatment.
Chlamydia is the most frequently reported STI in the U.S., with over 1.6 million cases documented in 2022. While many infected individuals remain asymptomatic, some experience symptoms such as painful urination, genital discharge, or rectal pain and bleeding. Untreated chlamydia can lead to serious complications like pelvic inflammatory disease, arthritis, and infertility, and increases the risk of contracting other STIs.
The mystery of chlamydia recurrence, even after seemingly effective antibiotic treatment, has puzzled researchers for some time. Genetic analysis of recurring infections often reveals strains nearly identical to the original infection, suggesting more than simple reinfection. While factors like incomplete treatment, repeated exposure to an untreated partner, or contaminated sex toys can contribute to recurrence, some studies hint at a hidden reservoir within the body where chlamydia bacteria can persist.
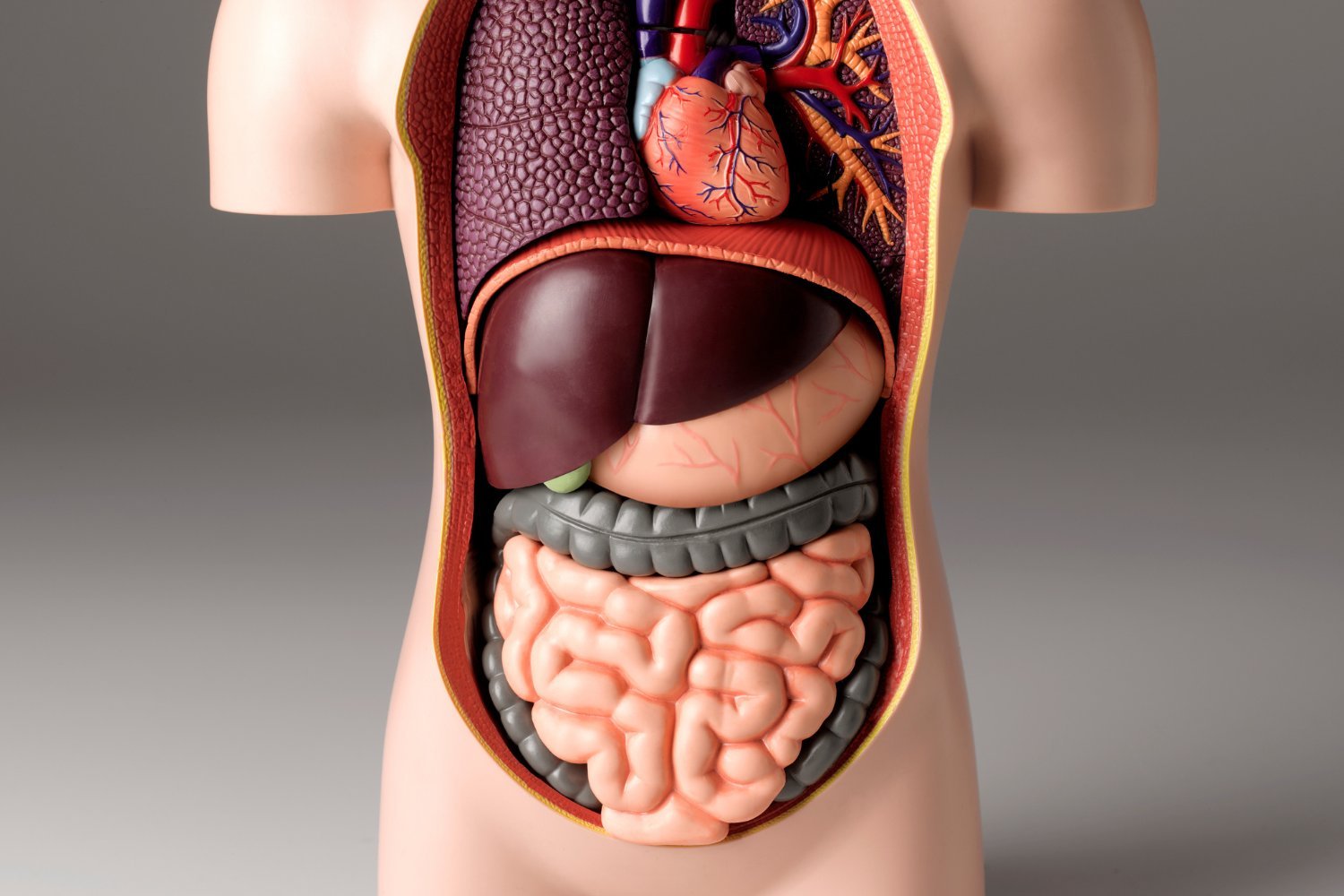
Related chlamydia species are known to inhabit the guts of their hosts, leading scientists to investigate the human gut as a potential hiding place for C. trachomatis. A recent study published in PLOS Pathogens offers compelling evidence to support this theory. Researchers at the University of Würzburg in Germany utilized human gut organoids – miniature, lab-grown versions of gut tissue – to study chlamydia infection. They discovered that while the bacteria struggled to infect the organoids’ outer “apical” surface, they readily infected the “basolateral” surface, which connects to underlying tissues and blood vessels.
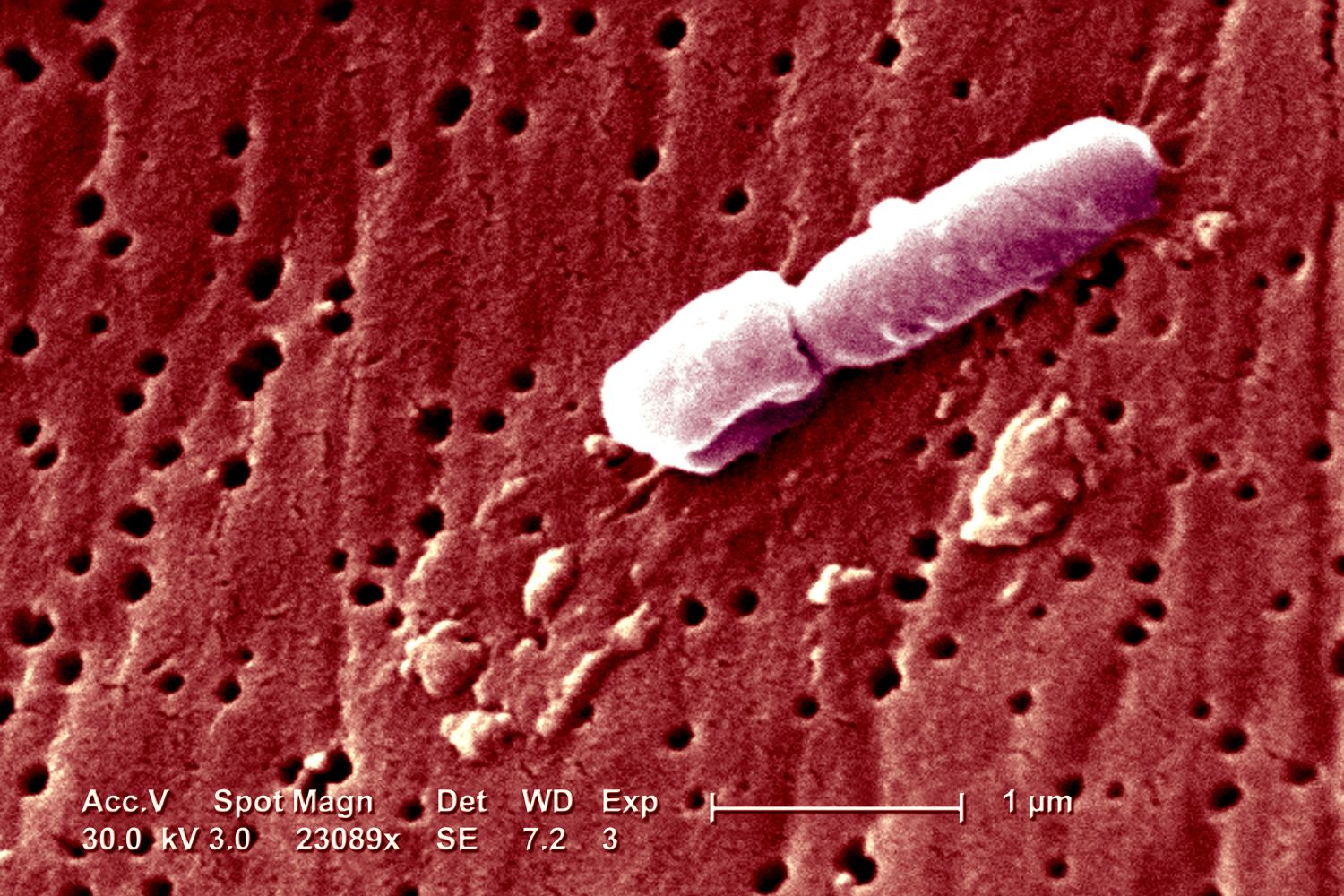
Further examination of the infected organoids revealed the presence of persistent forms of chlamydia bacteria, identifiable by their distinct shape under an electron microscope, according to lead researcher Pargev Hovhannisyan. While this research doesn’t definitively prove chlamydia’s ability to persist in the human gut, it significantly strengthens the hypothesis. Further research is needed to confirm these findings and understand how chlamydia reaches the gut and which specific cells it targets.
This potential discovery underscores the complexity of chlamydia and highlights the need for continued research. However, it doesn’t change current recommendations for STI prevention. Regular testing for chlamydia and other STIs, consistent condom use, and completing prescribed antibiotic treatments remain crucial. Early detection and proper treatment are essential for preventing long-term health consequences.
This new research suggests a possible explanation for recurrent chlamydia infections, potentially impacting future treatment strategies. While further investigation is necessary, the findings reinforce the importance of safe sex practices and regular STI testing.