Fat cells, often seen as a health concern, may hold a surprising key to fighting cancer. A recent study published in Nature Biotechnology by researchers at the University of California, San Francisco (UCSF) reveals how engineered beige fat cells can starve tumors and inhibit their growth. This breakthrough could potentially revolutionize cancer treatment with a relatively simple and accessible approach.
Our bodies contain three primary types of fat cells: white, brown, and beige. White fat cells store energy, while brown fat cells regulate body temperature by burning sugar and fat when we’re cold. Beige fat cells possess the unique ability to function as either white or brown fat cells as needed.
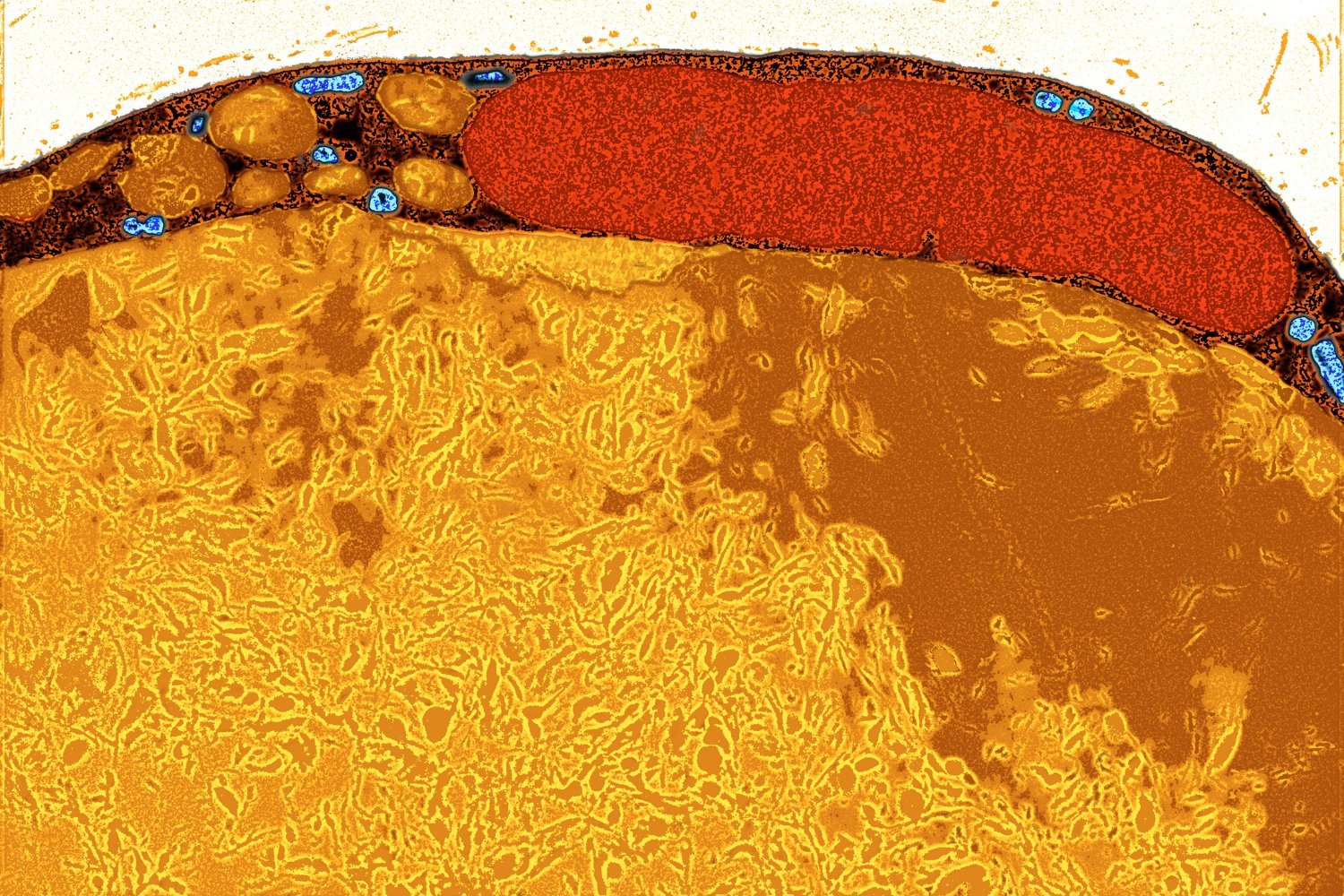
Previous research indicated that cold-induced brown fat cells could deprive cancer cells of the resources they need to grow. However, brown fat cells are scarce, and cold therapy presents safety concerns for many cancer patients. The UCSF researchers aimed to replicate this anti-tumor effect safely by converting white fat cells into beige fat cells – a transformation scientists are increasingly mastering.
Utilizing CRISPR gene-editing technology, the researchers targeted the UCP1 gene to reprogram white fat cells into beige fat cells. In some cases, the cells were further modified to prioritize nutrients that certain cancers aggressively consume.
Through experiments involving petri dishes, mice, and human patient samples, the engineered beige fat cells demonstrated a remarkable ability to suppress cancer growth. The cells effectively countered at least five different types of cancer: colon, pancreatic, prostate, and two types of breast cancer. Impressively, the treatment showed promise even when the fat cells were implanted at a distance from the tumors.
As the researchers noted in their paper, these results provide a strong foundation for a novel cancer therapeutic approach—adipose manipulation transplantation—which can be personalized for specific cancers and patients.
While these findings are preliminary, they offer significant potential. Further research is needed to validate and expand upon these results before this approach can be considered a viable cancer treatment. However, the researchers are optimistic about the feasibility and practicality of this experimental therapy. Body fat is readily available, and medical professionals are already skilled in fat removal and transplantation procedures.
“We already routinely remove fat cells with liposuction and put them back via plastic surgery,” explains Nadav Ahituv, Director of the UCSF Institute for Human Genetics. “These fat cells can be easily manipulated in the lab and safely placed back into the body, making them an attractive platform for cellular therapy, including for cancer.”
Looking ahead, the research team envisions a future where engineered fat cells not only treat cancer but also perform other beneficial functions, such as monitoring blood glucose levels or removing excess iron. This exciting new avenue of research could transform how we approach disease treatment and improve patient outcomes.
https://www.nature.com/articles/s41587-024-02551-2
https://www.nih.gov/news-events/nih-research-matters/how-brown-fat-improves-metabolism
https://www.nature.com/articles/s41392-022-01284-5
https://www.ucsf.edu/news/2025/01/429411/how-hungry-fat-cells-could-someday-starve-cancer-death