Immunotherapy has revolutionized cancer treatment, but not all patients respond. A new study suggests fecal microbiota transplants (FMT) could enhance the effectiveness of immunotherapy in patients with advanced gastrointestinal cancers who have developed resistance to standard treatments. This groundbreaking research offers hope for a combination therapy approach to some of the most challenging cancer cases.
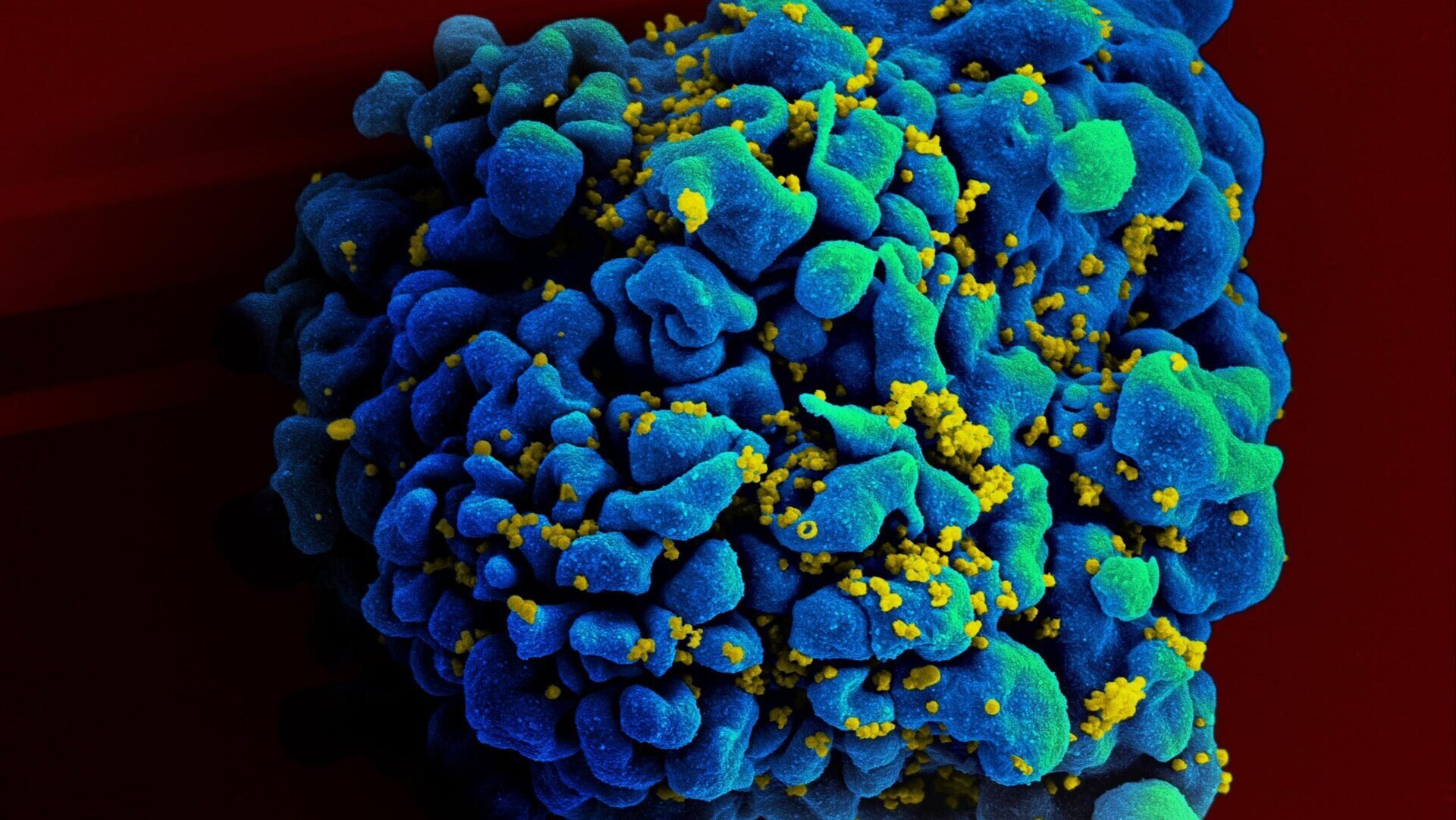
Immune checkpoint inhibitors, a cornerstone of immunotherapy, target proteins that prevent the immune system from recognizing and attacking cancer cells. While highly effective for some, these inhibitors are not universally successful, and some patients develop resistance. Emerging research points to the gut microbiome, the complex community of bacteria residing in our digestive tract, as a key factor influencing immunotherapy response. This has led scientists to explore FMT as a potential strategy to re-engineer the gut microbiome and improve immunotherapy outcomes.
Previous research has demonstrated the potential of FMT in melanoma patients. This latest study, however, represents one of the first investigations into the efficacy of FMT in other types of metastatic solid tumors, specifically gastrointestinal cancers.
Thirteen patients with various gastrointestinal cancers, all exhibiting resistance to anti-PD-1 inhibitors, participated in the trial. They received FMT from donors who had responded positively to immunotherapy, followed by another round of anti-PD-1 treatment. Remarkably, half of the patients (six) showed a noticeable positive response, with five experiencing cancer stabilization.
The study, published in Cell Host & Microbe, suggests that FMT with beneficial microbiota can overcome resistance to anti-PD-1 inhibitors in advanced solid cancers, particularly those affecting the gastrointestinal tract. While these findings are preliminary and require further validation through larger-scale trials, they offer crucial insights into the intricate relationship between the gut microbiome and immunotherapy response. The researchers identified specific bacterial strains associated with both positive and negative responses to the inhibitors, paving the way for more targeted and personalized immunotherapy approaches.
Further research will focus on understanding the complex interactions within the microbiome to identify optimal microbial communities for enhancing cancer treatment outcomes. This comprehensive approach will shed light on how the microbial ecosystem as a whole contributes to therapeutic success. The ultimate goal is to develop personalized FMT protocols that maximize the effectiveness of immunotherapy and improve outcomes for patients with advanced gastrointestinal cancers and potentially other solid tumors.
The research underscores the potential of FMT to reshape the landscape of cancer treatment, offering a new avenue for enhancing immunotherapy effectiveness and addressing treatment resistance.