Your place of residence could play a more significant role in your brain’s aging process than previously understood. Groundbreaking research published recently indicates that the likelihood of a dementia diagnosis varies considerably across different regions of the United States, pointing to complex underlying factors that influence US dementia risk. This pivotal study, led by scientists at the University of California, San Francisco (UCSF), and featured in JAMA Neurology, analyzed veteran medical records to uncover these striking geographical patterns.
Dementia’s Expanding Impact on Public Health
Dementia represents a rapidly escalating public health challenge, particularly impacting the aging population. Currently, over six million Americans are living with dementia. Furthermore, a government-funded study highlighted by the National Institutes of Health in February projected a sobering statistic: 42% of Americans over the age of 55 are expected to develop dementia within their lifetime. The condition is complex, typically arising from an interplay of environmental and genetic factors.
Landmark Study Uncovers Regional Dementia Patterns
Despite the growing prevalence of dementia, there has been limited research examining how dementia risk might differ geographically on a national scale, according to Dr. Kristine Yaffe, senior study author, neurologist, and chief of neuropsychiatry at the San Francisco VA healthcare system. Dr. Yaffe and her team identified a unique opportunity to investigate this using deidentified records from the Veterans Health Administration (VHA), the largest integrated healthcare system in the U.S.
“We realized the VA national data would allow for such an investigation as the VA has a uniform way of capturing data across the U.S.,” Dr. Yaffe explained to maagx.com. “There are no other national healthcare systems that have this.”
The research team meticulously studied the health records of over 1.2 million randomly selected VA patients aged 65 and older who had no pre-existing dementia. These individuals were monitored for an average of 12 years.
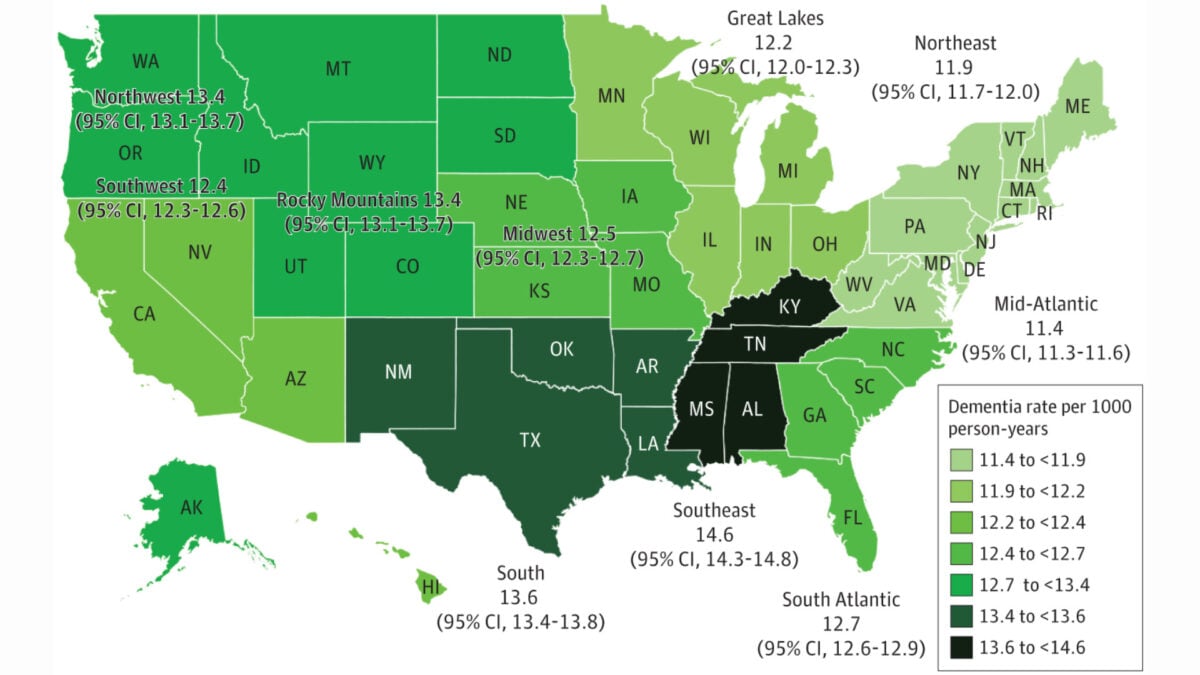
The findings were striking. After adjusting for age, the Mid-Atlantic region (encompassing states like Pennsylvania, Maryland, and Virginia) exhibited the lowest dementia rates. Using this region as a baseline, the researchers discovered significantly higher rates elsewhere:
- Southeast (Kentucky, Tennessee, Alabama): 25% higher
- Northwest (Idaho, Oregon, Washington) and Rocky Mountains (Colorado, Montana, the Dakotas): 23% higher for both
- South (Texas, New Mexico, Louisiana): 18% higher
- Southwest (California, Nevada, Arizona): 13% higher
- Northeast (New York): 7% higher
“This is a very large difference, especially given that these are all veterans with care at the VAHS,” Dr. Yaffe commented. “It was really surprising we saw such big differences.”
Investigating the Roots of Regional Dementia Variation
The research team initially hypothesized that factors such as average education levels, the rurality of a state, or the prevalence of other health conditions like heart disease might account for these regional variances. However, even after adjusting their models for these variables, the observed patterns in dementia rates remained largely unchanged.
This persistence suggests that other, perhaps less tangible, factors could be at play – elements not easily captured through standard medical records alone. It implies that fundamental differences may exist that predispose individuals in certain regions, like Kentucky, to a higher dementia risk compared to similar individuals in states like New Jersey, which falls within the lower-risk Mid-Atlantic region.
Dr. Yaffe posited potential explanations: “It’s possible that the differences are explained by lifelong differences in things like education quality (vs quantity) and social determinants of health might be driving some of the differences.” Social determinants of health encompass a wide range of non-medical factors that influence health outcomes, including socioeconomic status, access to quality education and healthcare, community environment, and social support networks.
Conclusion: Charting a Course for Future Prevention
This comprehensive study compellingly demonstrates significant and, as yet, unexplained regional disparities in dementia risk across the United States. The findings underscore the urgent need for further research to delve into the complex, deep-seated factors contributing to these geographic differences. Unraveling these underlying causes is not merely an academic exercise; it holds the potential to unlock new, targeted strategies for dementia prevention and ultimately improve brain health outcomes for aging populations nationwide. The lessons learned could pave the way for interventions that address specific regional vulnerabilities.
References
- Kaup, A. R., Xia, F., Tan, Z. S., et al. (2024). Geographic Variation in Dementia Risk in a National Cohort of US Veterans. JAMA Neurology. Published online April 29, 2024. doi:10.1001/jamaneurol.2024.0805
- National Institutes of Health. (2024, February). Risk and future burden of dementia in the United States. NIH Research Matters. https://www.nih.gov/news-events/nih-research-matters/risk-future-burden-dementia-united-states