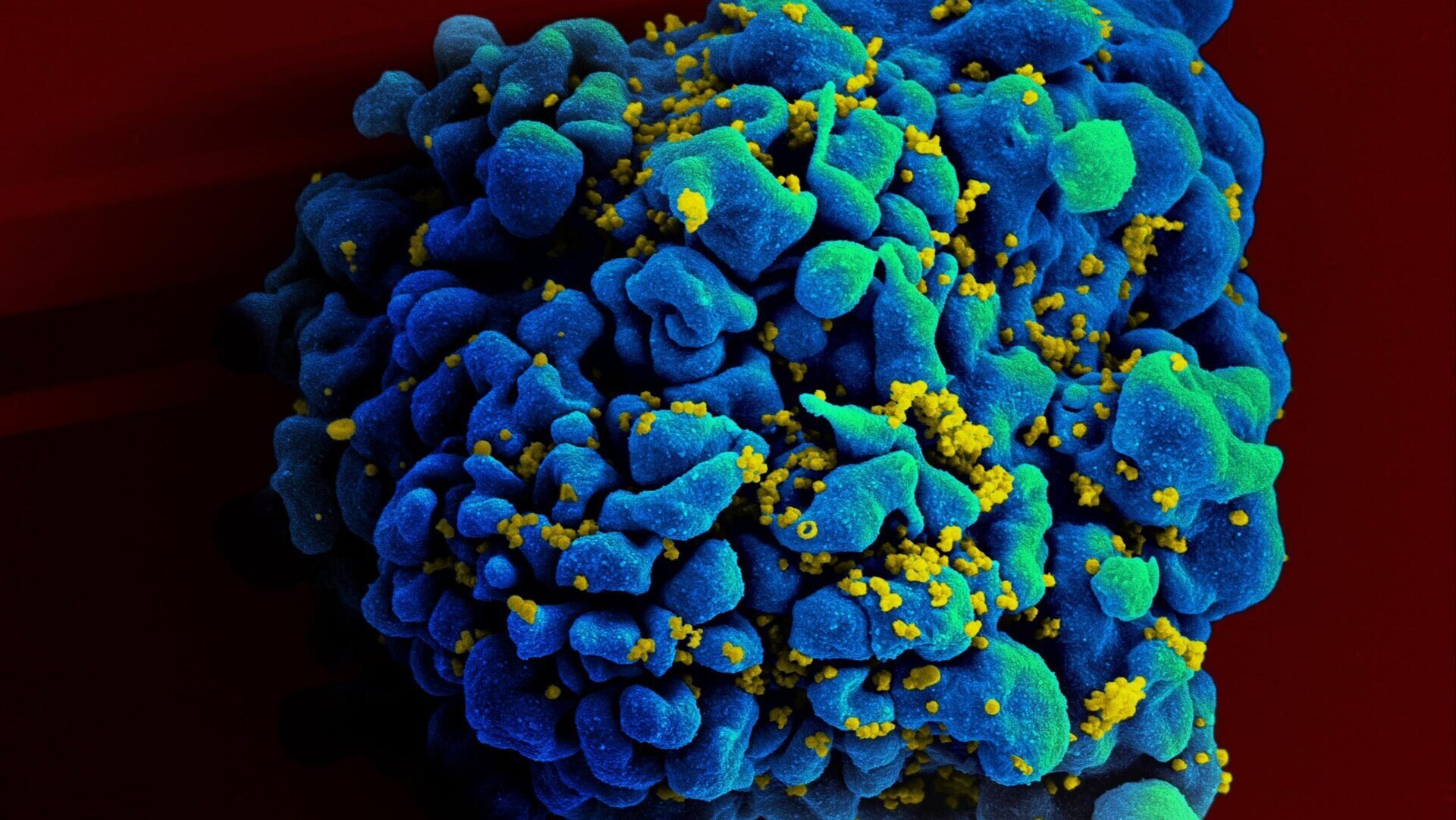
A 60-year-old man in Germany has become the seventh person reportedly cured of HIV following a bone marrow transplant. Remarkably, this case differs from previous successes as the donor’s stem cells lacked the CCR5-delta 32 mutation, previously thought essential for achieving HIV remission through this method. This breakthrough offers new insights into HIV treatment and potential cure strategies.
The patient, diagnosed with HIV in 2009, later developed acute myeloid leukemia (AML) in 2015. A bone marrow transplant was recommended to treat the AML. This procedure, performed at Charité Universitatsmedizin Berlin, essentially replaces the patient’s immune system with the donor’s. This same hospital facilitated the first successful HIV cure via bone marrow transplant in 2007, known as the “Berlin Patient” (Timothy Ray Brown). Like Brown, this latest patient, dubbed the “next Berlin Patient,” has chosen to remain anonymous.
Previous successful transplants utilized donors with two copies of the CCR5-delta 32 mutation. This mutation alters the CCR5 receptor on white blood cells, making them resistant to HIV-1 infection. Transferring these resistant cells was believed crucial for eradicating the virus. However, in this case, a compatible donor possessing only one copy of the mutation was available. Surprisingly, the transplant proved successful. The patient ceased HIV medication in 2018, and subsequent tests have revealed no detectable virus, indicating a potential cure. He also remains cancer-free.
The case was presented at AIDS 2024, the 25th International AIDS Conference. In a statement released by the International AIDS Society, the patient expressed, “A healthy person has many wishes, a sick person only one.”
The precise mechanism behind this cure remains unclear. Individuals with a single CCR5-delta 32 mutation can still contract HIV, although their risk may be reduced. It’s possible that even one copy of the mutation contributes to viral elimination. Another theory suggests that replacing the entire immune system, regardless of the CCR5 mutation, could be sufficient. However, other HIV patients receiving transplants from donors without the mutation experienced viral rebound, indicating other factors might be at play.
Bone marrow transplants are a high-risk procedure with potentially life-threatening side effects, reserved for severe conditions like leukemia. With effective antiretroviral therapies controlling HIV and preventing transmission, transplants are unlikely to become a standard HIV cure. However, this case provides valuable insights that could inform the development of more practical cures, including gene therapy approaches.
Sharon Lewin, president of the International AIDS Society, stated, “The next Berlin Patient’s experience suggests that we can broaden the donor pool for these kinds of cases…This is also promising for future HIV cure strategies based on gene therapy because it suggests that we don’t have to eliminate every single piece of CCR5 to achieve remission.”
While bone marrow transplants are not a viable solution for most people living with HIV, this case offers hope and direction for future research into more accessible and less invasive cure strategies.