Traumatic brain injuries (TBIs) are a significant public health concern, affecting hundreds of thousands of people annually and often leading to long-term neurological issues. While current treatments focus on managing acute symptoms, there’s a critical need for therapies that can prevent chronic complications. A recent study published in Nature Neuroscience offers a glimmer of hope, suggesting a nasal spray containing an antibody could potentially reduce brain damage following a TBI.
Researchers at Mass General Brigham tested an experimental antibody-based nasal spray, called foralumab, on mice with brain injuries. The results indicated the spray may enhance the brain’s natural healing process while simultaneously mitigating harmful inflammation. This dual action could pave the way for a preventative treatment against the long-term effects of TBIs, strokes, and other neurological conditions.
According to the Centers for Disease Control and Prevention (CDC), TBIs result in a substantial number of hospitalizations and fatalities each year. Furthermore, research increasingly links even mild TBIs, such as concussions, to persistent neurological problems and a potentially elevated risk of dementia later in life. Current treatments, like rest for concussions or surgery for severe injuries, primarily address immediate damage. No established medication exists to prevent the chronic consequences, although rehabilitation therapy plays a crucial role in recovery.
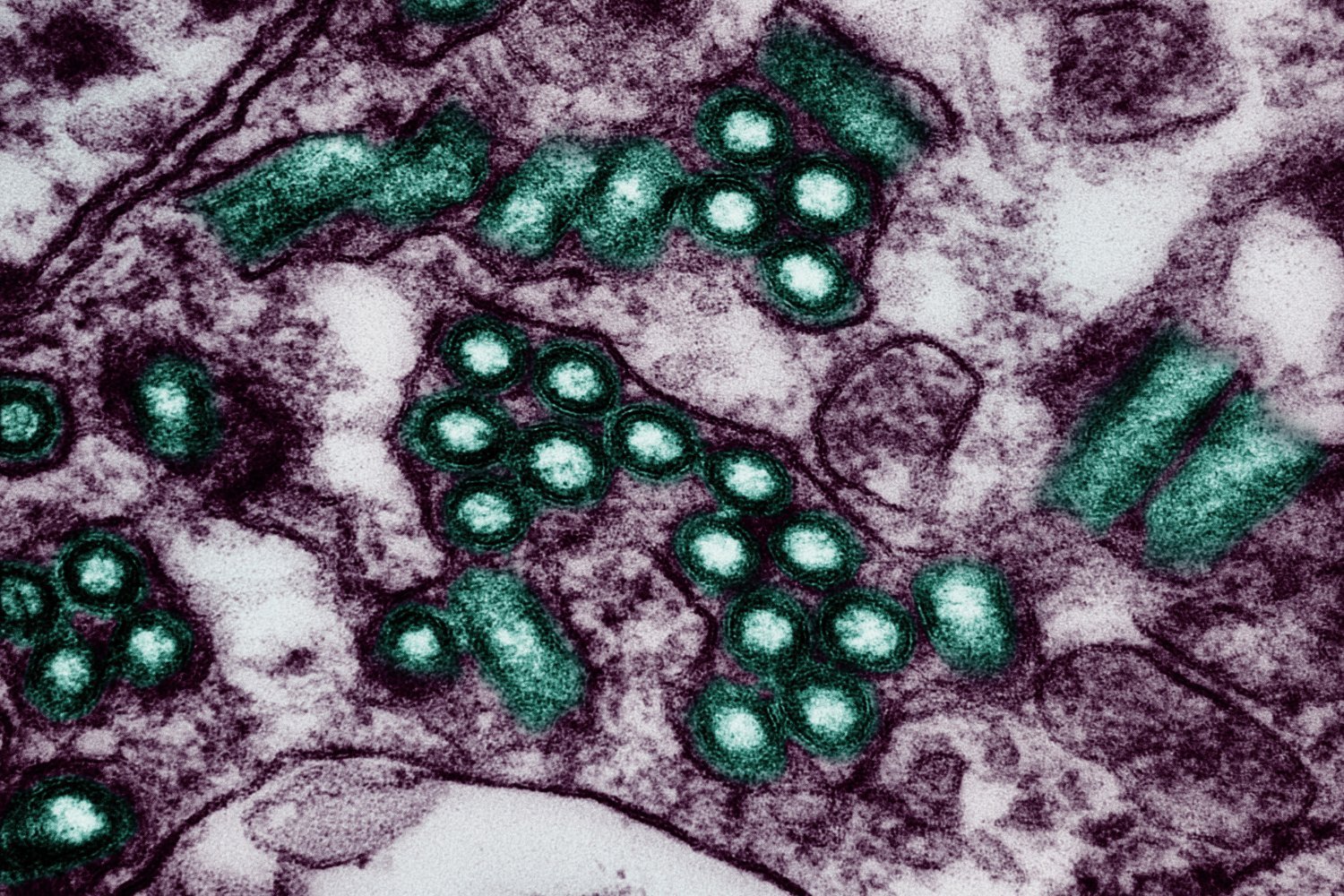
The Mass General Brigham researchers have been exploring foralumab, developed by Tiziana Life Sciences, for its potential in treating neurological conditions like multiple sclerosis. The antibody targets CD3, a protein group interacting with the brain’s immune cells. Previous research suggests that suppressing CD3 can boost the activity of regulatory T cells (Tregs), which help regulate the brain’s immune response and prevent excessive inflammation.
Lead researcher Saef Izzy, head of the Immunology of Brain Injury Program at Brigham and Women’s Hospital, emphasized the devastating impact of TBIs, highlighting chronic inflammation as a key contributor to long-term disability and cognitive decline. In the mice study, foralumab, by increasing Treg cell activity, appeared to improve the brain’s immediate healing response after injury. Specifically, the treated mice showed enhanced microglia function, the brain’s primary immune defense, in clearing damaged cells. The treatment also seemed to prevent chronic microglia inflammation. Consequently, mice treated with foralumab within three days of injury demonstrated greater improvements in motor function and coordination compared to the control group.
The researchers concluded that nasal anti-CD3, like foralumab, represents a promising new therapeutic approach for TBI and potentially other acute brain injuries. While these findings are encouraging, further research is essential to confirm the drug’s efficacy in humans. Foralumab has already shown early promise in human trials for multiple sclerosis, and trials for Alzheimer’s and amyotrophic lateral sclerosis are either ongoing or planned. These developments offer hope that this antibody could become a valuable treatment option for a range of brain conditions, including TBI.