Shingles, a painful reactivation of the chickenpox virus, can have lasting health consequences. A new study published in Nature Medicine suggests the Shingrix shingles vaccine may offer an additional benefit: a reduced risk of dementia. While more research is needed to confirm a direct causal link, the findings highlight a potential connection between shingles vaccination and cognitive health.
Shingles, also known as herpes zoster, occurs when the varicella-zoster virus (VZV), the same virus responsible for chickenpox, reactivates later in life. After a childhood bout of chickenpox, VZV lies dormant in the nervous system. For about one-third of individuals, the virus reemerges, causing the painful rash and nerve inflammation characteristic of shingles. Symptoms can persist for weeks, and some individuals experience chronic nerve pain (postherpetic neuralgia) for months or even years.
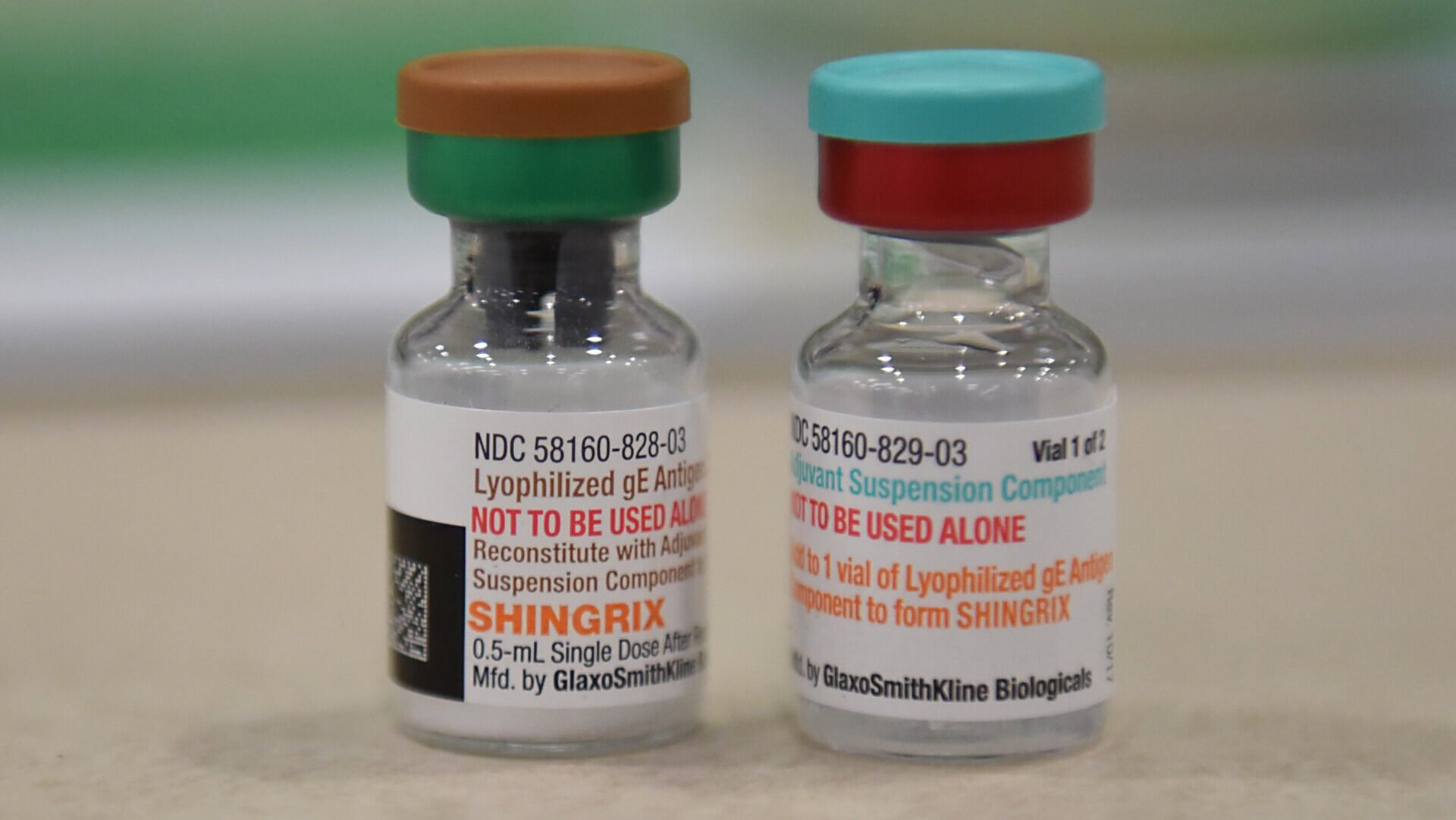
Two vaccines are available to prevent shingles: Zostavax and the more recent Shingrix. Shingrix, approved in 2017, boasts over 90% efficacy and longer-lasting protection compared to Zostavax. Its recombinant formulation, using specific viral components rather than a weakened live virus, makes it safe for immunocompromised individuals. Shingrix is currently the only shingles vaccine available in the U.S., recommended for adults over 50.
Could Shingrix Protect Against Dementia?
Previous research hinted at a possible link between Zostavax and a lower dementia risk. However, studies on Shingrix have been limited. The new Nature Medicine study aimed to address this gap. Researchers analyzed health records of over 200,000 individuals vaccinated for shingles, comparing Shingrix recipients to those who received Zostavax and other common vaccines like the flu and tetanus/diphtheria/pertussis (Tdap) shots.
Over a six-year period, individuals vaccinated with Shingrix demonstrated a 17% lower risk of developing dementia compared to the Zostavax group. They also exhibited a lower dementia risk than those who received the flu or Tdap vaccines. Furthermore, among those who did develop dementia, Shingrix vaccination was associated with an estimated six-month delay in symptom onset compared to Zostavax.
Further Research is Crucial
While promising, these observational findings don’t definitively prove that Shingrix prevents or delays dementia. The underlying mechanisms remain unclear. Some research suggests certain pathogens, including herpesviruses like VZV, could directly contribute to dementia development. However, this connection requires further investigation.
The study authors emphasize the need for more robust research to confirm these initial findings. Future studies should explore the biological mechanisms behind this potential protective effect and conduct randomized controlled trials to definitively establish the relationship between Shingrix and dementia risk. This research could potentially pave the way for new strategies to prevent or delay cognitive decline.
In conclusion, while the observed association between Shingrix and lower dementia risk is encouraging, it’s crucial to remember that correlation doesn’t equal causation. Further research is necessary to validate these findings and explore the potential mechanisms involved. However, the study highlights the importance of shingles vaccination and its potential benefits beyond simply preventing the painful rash.