Type 1 diabetes affects millions worldwide, requiring lifelong insulin management. A groundbreaking phase I clinical trial in China offers a glimmer of hope for a potential cure using stem cell therapy. Researchers successfully transformed a patient’s own stem cells into insulin-producing pancreatic cells, effectively replacing the damaged cells responsible for the disease.
Type 1 diabetes, an autoimmune disease, occurs when the body’s immune system mistakenly attacks the insulin-producing islet cells in the pancreas. Unlike the more prevalent type 2 diabetes, type 1 diabetes requires regular insulin injections to manage blood sugar levels. Although manageable, it can significantly impact life expectancy and quality of life. This new research presents a potential game-changer for those living with this chronic condition.
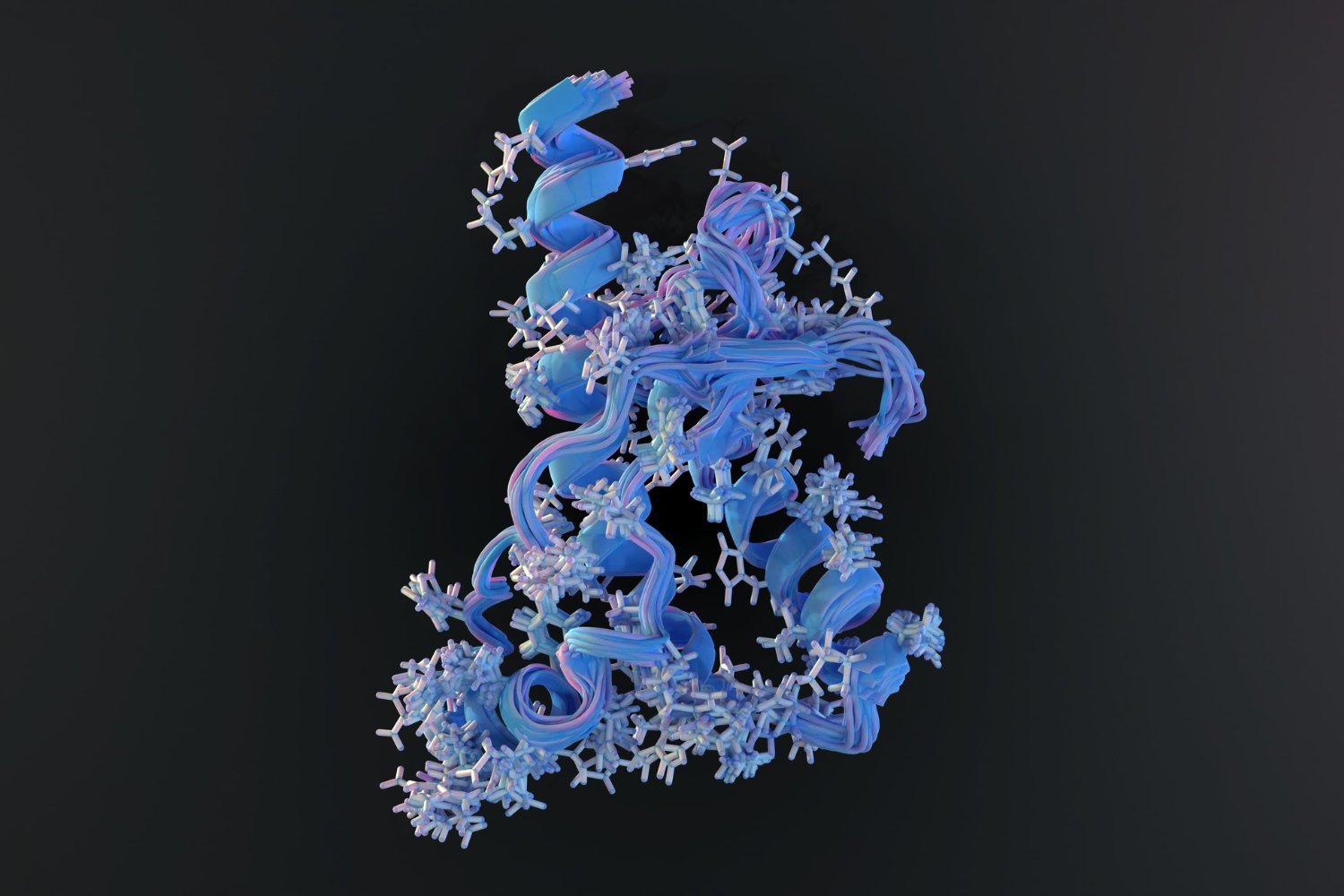
The Chinese research team conducted a small, yet significant, phase I clinical trial involving three patients with type 1 diabetes. The process involved extracting cells from the patients and converting them into pluripotent stem cells – cells capable of developing into various cell types. These pluripotent stem cells were then chemically induced to mature into insulin-producing pancreatic islets, mirroring the cells destroyed by the immune system in type 1 diabetes. These newly created islets were then transplanted into the patients’ abdomens. This location was chosen for easier monitoring and potential removal if complications arose.
The researchers published their one-year findings on the first patient, a 25-year-old woman, in the journal Cell. Remarkably, just 75 days after the procedure, the woman began producing enough insulin to discontinue her injections. Within four months, her long-term glucose levels normalized, resembling those of a non-diabetic individual. A year later, she continued to produce insulin, maintaining healthy blood sugar levels without any transplant-related complications. Stem cell derived islets transplantation
While these initial results are incredibly promising, it’s crucial to remember they are preliminary. Phase I trials primarily focus on assessing the safety of a treatment, not necessarily its efficacy. The history of stem cell research is marked by both exciting breakthroughs and subsequent setbacks, underscoring the need for cautious optimism. Furthermore, the trial participant was already taking immunosuppressants due to a prior liver transplant. This raises questions about the treatment’s long-term success in individuals without pre-existing immunosuppression, as their immune systems could potentially reject the transplanted islets. Long-term blood glucose control
Despite these caveats, if these positive outcomes are replicated in the remaining two trial participants and subsequent larger clinical trials, this stem cell therapy could revolutionize type 1 diabetes treatment. It holds the potential to provide a functional cure for a debilitating and life-altering condition, offering hope for a future free from daily insulin injections.
Further research is needed to confirm the long-term effectiveness and safety of this approach. Scientists must investigate the treatment’s impact on individuals with varying medical histories and without pre-existing immunosuppression. However, this initial success marks a significant step forward in the pursuit of a cure for type 1 diabetes, offering a beacon of hope for millions affected by this disease.